Finding Cancer Screening Messages That Resonate

Colorectal cancer is the third most common cancer in the United States and one of the top causes of cancer deaths. Screening can help reduce deaths from colorectal cancer by catching abnormal growths in the colon before they spread or before they become cancerous. But only about two-thirds of U.S. adults ages 50 to 75—the range for which the procedure is recommended—get screened for these growths. 1 Some demographic populations, including Latinos, people without health insurance, and people who have been in the United States for less than 10 years, are even less likely to be screened.
Researchers with the Participatory Research to Advance Colon Cancer Prevention (PROMPT) study are working to increase colorectal cancer screening rates for Latinos. The researchers collaborated with Latino community members in Southern California to create culturally appropriate materials to inform patients about colorectal cancer screening. Now the researchers are using the materials in a study to find an optimal schedule for contacting people and reminding them to do their annual colorectal cancer screening.
“For changing health behavior, such as encouraging people to get the recommended timely health screenings, research has shown that it is crucial to frame the health messages in terms that people understand and can relate to,” says Dr. Rina Das, scientific program officer at the National Institute on Minority Health and Health Disparities (NIMHD). “Incorporating participant feedback through community based participatory research (CBPR) approaches to adapt culturally relevant health messages helps close the health disparities gap and reach NIMHD’s vision of a future in which everyone has an equal opportunity to live a long, healthy, and productive life.”
Detecting Colorectal Cancer
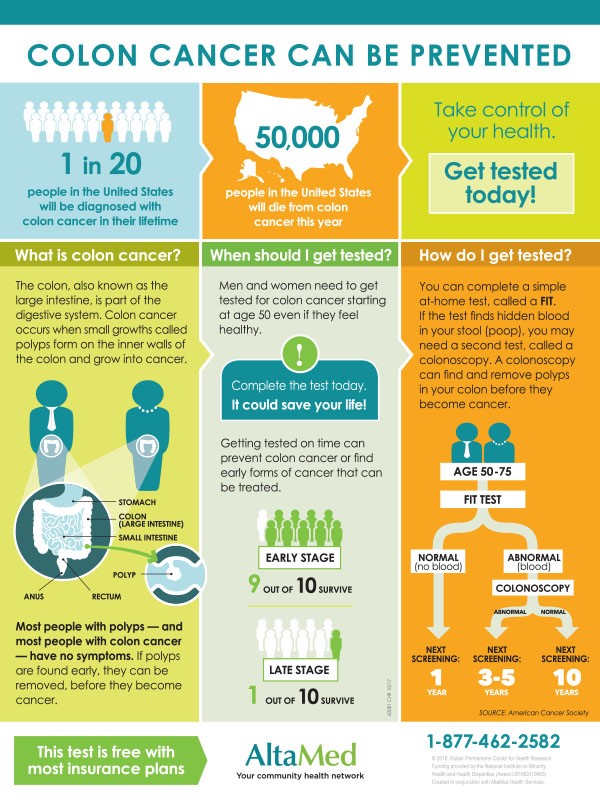
Colorectal cancer is cancer of the bottom part of the digestive system—the colon, also known as the large intestine, and the rectum. Colorectal cancer kills more than 50,000 people each year in the United States. 2
Screening can help reduce deaths from colorectal cancer. One form of screening for colorectal cancer is a colonoscopy, in which a doctor examines the inside of the colon and rectum by using a colonoscope,. However, colonoscopies are inconvenient; you have to take time off work, take strong laxatives to empty out your colon, and get someone to drive you home from the appointment because of the sedation used for the procedure.
Another method is the fecal immunochemical test, or FIT, which is convenient and can be done at home. For the FIT, you place a small sample of feces on a card and return it to the doctor for testing. “Data show that patients are more likely to get screened if they can do so with a FIT,” says Gloria Coronado, Ph.D., the leader of the study and a researcher at the Center for Health Research at Kaiser Permanente Northwest in Portland Oregon. In addition, she notes, research has shown that an annual FIT is just as good at preventing colorectal cancer as a once-a-decade colonoscopy. But getting patients to actually collect a sample and send in the card every single year is a challenge. In FIT outreach programs, a FIT card is mailed to each person who needs screening.
Involving Community Members
The researchers worked with AltaMed, a large health center with 35 clinics in Los Angeles and Orange counties, California. The center is the largest federally qualified health center in the country. Federally qualified health centers receive government funding to provide health care in underserved areas. More than 80% of AltaMed’s patients are Latino. Coronado’s own father was a Mexican immigrant and a farmworker. While there are already many researchers who study cancer, she says, there is much more to learn, particularly in diverse populations. “There need to be more people doing cancer research among people facing health literacy barriers.”
Coronado and her colleagues wanted to develop messages to persuade Latinos to return their FIT tests. To do this, they used a method called Boot Camp Translation, developed by researchers in Colorado. 3
“In the past, we’ve relied on focus groups to get feedback on messages,” Coronado says. In focus groups, the patients are not expected to know anything about a topic. “The reason I like Boot Camp Translation is that it really intends to make the patients experts in a given topic area.” The “translation” part of the method is about tailoring materials to an audience, not translating the text into another language.
AltaMed staff recruited 25 participants. All were Latinos ages 50 to 75, and they were split into two groups based on their language preference: either Spanish or English. Each group came together for an all-day meeting. The meetings kicked off with two expert presentations from Coronado: one about colorectal cancer and one catching participants up on results from the handful of studies that have tested messages about colorectal cancer screening. The participants were interested and engaged, Coronado said: “They had tons of questions.” Each group worked together to focus the messaging and continued refining the materials through a series of three teleconferences.
Materials and Messaging
The materials developed by the groups included a follow-up letter sent after the FIT is mailed, a fact sheet about colorectal cancer and colorectal cancer screening, and scripts for texts and phone calls. The researchers were prepared to use different materials for English- and Spanish-language contacts, but in the end, the groups had such similar recommendations that they were able to use materials with the same messages in their respective languages. The materials they developed are free for anyone to use and modify. 4
Participants were enthusiastic about statements like “‘I really want you to get tested and here’s why’—they loved that personal ‘I’ statement,” Coronado says. The participants wanted to stress the urgency of screening by sending out a reminder relatively soon after the test was sent. They also wanted to emphasize that the test is free. Participants liked the idea of focusing on family ties and loved the family photo included in the introduction letter.
Optimizing the Schedule
In addition to creating the materials, the participants came up with a schedule of when they would want text messages, phone calls, and other notifications about the FIT. The researchers used this schedule and the new materials for a pilot study, conducted at two AltaMed clinics. In this study, which included 1,767 patients, the researchers found that both live and automated phone calls increased the chance that someone would return their FIT. Live phone calls were particularly effective, but they are also the most expensive way to reach patients, so the researchers suggested that it might be best to save them for the people who are the least likely to return their FIT cards. 5
Based on the results of the pilot, the researchers are now running a larger study, testing a combination of live and automated calls with more patients, at 15 clinics that are part of AltaMed.
References
- https://www.cdc.gov/cancer/colorectal/statistics/index.htm
- https://www.cdc.gov/cancer/colorectal/statistics/index.htm
- Norman, N., Bennett, C., Cowart, S., Felzien, M., Flores, M., Flores, R., . . . Westfall, J. M. (2013). Boot camp translation: a method for building a community of solution. Journal of the American Board of Family Medicine, 26(3), 254-263. doi:10.3122/jabfm.2013.03.120253
- Thompson, J. H., Davis, M. M., Michaels, L., Rivelli, J. S., Castillo, M. L., Younger, B. M., . . . Coronado, G.D. (2019). Developing patient-refined messaging for a mailed colorectal cancer screening program in a Latino-based community health center. Journal of the American Board of Family Medicine, 32(3), 307-317. doi:0.3122/jabfm.2019.03.180026
- Coronado, G. D., Thompson, J. H., Petrik, A. F., Nyongesa, D. B., Leo, M. C., Castillo, M., . . . Chen, A. (2019). Patient-refined messaging for a mailed colorectal cancer screening program: Findings from the PROMPT study. Journal of the American Board of Family Medicine, 32(3), 318-328. doi:10.3122/jabfm.2019.03.180275
Posted October 9, 2019

















